Introduction
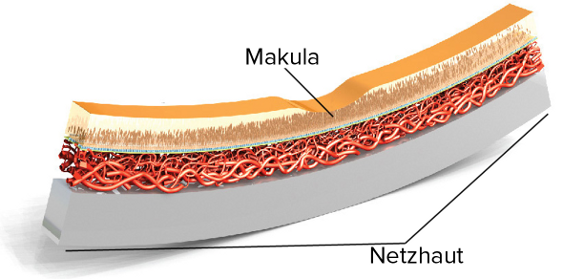
Die altersabhängige Makuladegeneration (AMD) ist in den westlichen Industrieländern die Hauptursache für Erblindung bei Menschen über 65 Jahren, weltweit sind über 30 Millionen Menschen betroffen. Die Sehfähigkeit im zentralen Gesichtsfeld geht durch das schrittweise Absterben von Netzhautzellen in der Makula verloren—dem Punkt des schärfsten Sehens‘. Mit der AMD sind selbst alltägliche Handlungen schwierig, so wie z.B. Lesen, Autofahren, Gesichter erkennen, Fernsehen oder Treppensteigen.
Die AMD ist nicht schmerzhaft und schreitet unterschiedlich voran, manchmal langsam, manchmal rasch, manchmal an einem Auge, manchmal an beiden. Wenn AMD sehr langsam beginnt, passt sich das Gehirn zuerst an, und die Symptome der Erkrankung sind oft schwer zu erkennen. Schreitet die Krankheit jedoch rasch voran, so macht sich der Verlust der Sehfähigkeit schnell bemerkbar. Unabhängig davon ob sich AMD langsam oder rasch entwickelt, führt das späte Stadium ohne Behandlung zum irreversiblen Verlust der Sehkraft.
Die AMD wird in zwei Formen eingeteilt: die trockene und die feuchte.
Diabetes
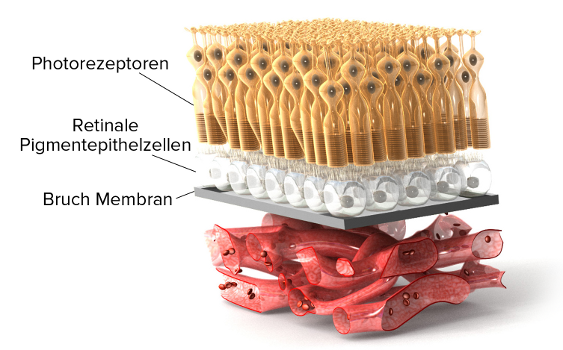
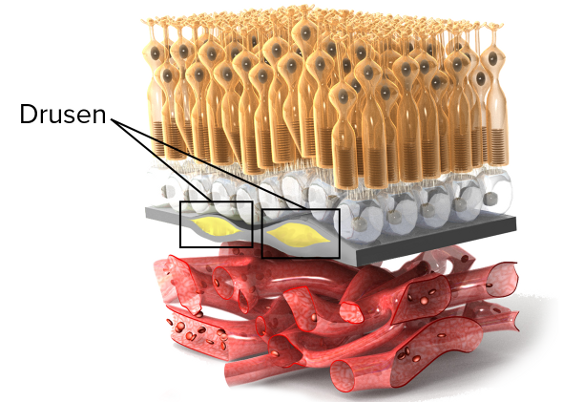
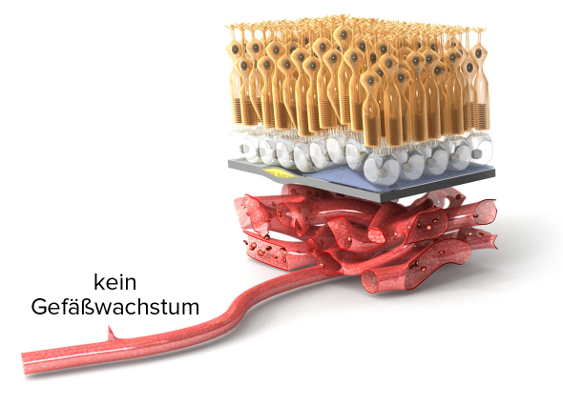
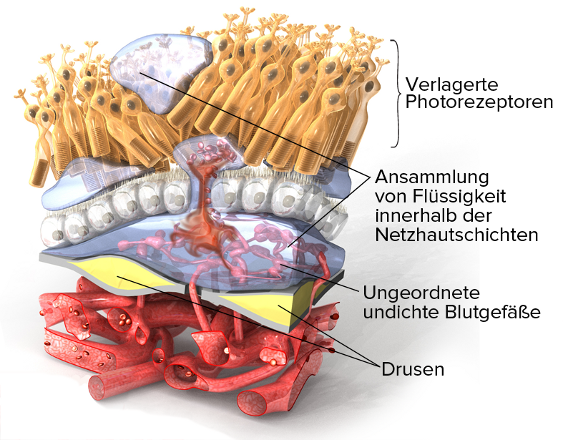
Die trockene AMD ist die häufigste Form von AMD, und stellt in den Anfangsstadien ca. 90% aller Fälle dar. Die trockene AMD beginnt mit einem Funktionsverlust der Netzhaut durch Ablagerungen von Drusen—das sind gelbe Ablagerungen im hinteren des Auges, in unterschiedlichen Größen und Anzahl, die meist als eine Begleiterscheinung des Alterns betrachtet werden. Zu Beginn der trockenen AMD bilden sich mehrere kleine Drusen oder wenige mittelgroße Drusen, aber die Patienten erleiden keinen Sehverlust. Das Frühstadium der trockenen AMD kann sich zum Zwischenstadium der trockenen AMD entwickeln, wenn sich weitere kleine Drusen oder eine oder mehrere große Drusen bilden. Die Begleiterscheinungen des Zwischenstadiums der trockenen AMD sind z.B. gewellte Linien oder verschwommene Flecken im Gesichtsfeld, sowie Schwierigkeiten beim Lesen.
Das Zwischenstadium der trockenen AMD kann sich entweder in ein fortgeschrittenes Stadium der trockenen AMD, oder aber zur feuchten AMD entwickeln. Bei der fortgeschrittenen trockenen AMD führt das ständige Wachstum der Drusen, in Anzahl und auch in Größe, zur Zerstörung der lichtempfindlichen Zellen der Netzhaut und des dort befindlichen Gewebes, was man « geographische Atrophie” nennt. Geografische Atrophie führt zu weiteren erheblichen und irreversiblen Störungen der Sehfähigkeit wie z.B. größere, dunklere Flecken in Sehzentrum, Abnahme des Kontrastempfindens, Abnahme der Anpassungsfähigkeit an veränderte Lichtverhältnisse, Abnahme der Lesefähigkeit für Kleingedrucktes.
Es können beide Augen oder nur eines von trockener AMD betroffen sein. Wenn nur ein Auge betroffen ist, ist der Sehverlust manchmal unbemerkbar da das gesunde Auge die Schwäche des kranken Auges korrigiert. Es ist also sehr wichtig, beide Augen regelmäßig untersuchen zu lassen.
Diabetic Retinopathy
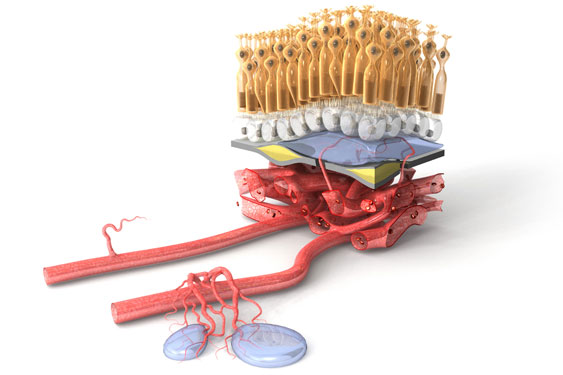
Die Feuchte AMD ist die schwerwiegendste und gravierendste Form von AMD und tritt erst im Spätstadium der Erkrankung auf. Alle Menschen mit feuchter AMD leiden vorerst unter trockener AMD, doch entwickelt sich die trockene AMD lediglich bei 10 bis 15% der Patienten zur feuchten Form. Ebenfalls unter „exsudative Makuladegeneration“ bekannt, bilden sich bei der feuchten AMD abnorme und meist undichte Gefäße unter der Makula.
Im Gegensatz zur trockenen AMD, die langsam und in Stadien fortschreitet, kann die feuchte AMD mitunter sehr rasch die Makula schädigen und zum Ausfall des zentralen Gesichtsfeldes führen. Deshalb ist es für Risikopatienten auch sehr wichtig, regelmäßig zum Augenarzt zu gehen.
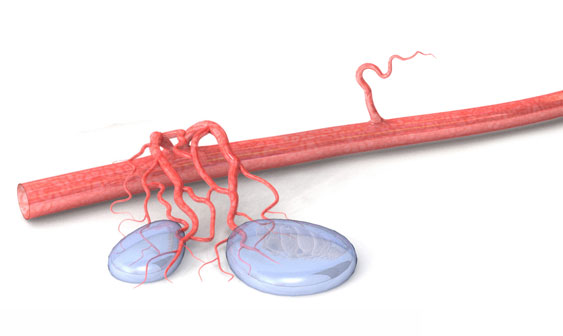
Bei der feuchten AMD bilden sich kleine Blutgefäße unter der Makula, auch als Angiogenese bezeichnet. Aus diesen neugebildeten Gefäßen treten Flüssigkeit und Blut aus, was zu einer blasenförmigen Verwölbung der Makula führen kann. Diese Wucherungen verzerren die Sehkraft im kranken Auge, und gerade Linien erscheinen verbogen. Es können ebenfalls einer oder mehrere dunkle Flecken im zentralen Gesichtsfeld erscheinen. Diese sind durch eine Ansammlung von Blut oder Flüssigkeit unter der Makula verursacht.
Ohne Behandlung können die Blutungen im Auge bei feuchter AMD zur Narbenbildung führen, wonach der damit verbundene Sehverlust irreversibel ist. Zum Glück gibt es mehrere wirksame Behandlungsmöglichkeiten gegen die feuchte AMD. Diese Therapien können das Fortschreiten des Krankheitsprozesses nicht nur aufhalten, sondern in manchen Fällen sogar das Sehvermögen verbessern, jedoch lediglich wenn die Gewebe noch nicht begonnen haben, sich zu vernarben.
Stages
Es gibt mehrere Risikofaktoren für AMD:
- Alter ist der größte Risikofaktor. Menschen über 60 Jahren sind am meisten gefährdet.
- Wenn nahe Familienmitglieder AMD haben, ist das Krankheitsrisiko erhöht.
- Wenn Sie AMD auf einem Auge haben, besteht ein hohes Risiko dass sich AMD auch im anderen Auge entwickelt.
- Raucher haben ein zwei- bis dreimal höheres AMD Risiko. Je mehr Sie rauchen, desto höher das Risiko. Das AMD Risiko verringert sich, wenn Sie aufhören zu rauchen.
- AMD ist bei Frauen weiter verbreitet als bei Männern.
- AMD ist bei Kaukasiern weiter verbreitet als bei Menschen afrikanischer Herkunft.
- Fettleibigkeit beschleunigt die Entwicklung des AMD Früh- oder Zwischenstadiums zur fortgeschrittenen AMD.
- Unkontrollierter Bluthochdruck erhöht ebenfalls das AMD Risiko.
Wie kann ich das Risiko verringern?
- Nicht rauchen
- Ein normales Körpergewicht beibehalten
- Den Blutdruck kontrollieren
- Eine Ernährung mit viel dunkelgrünem Blattgemüse und Obst verringert das AMD Risiko. Essen Sie regelmäßig Fisch und vermeiden Sie andere Fette. Diese Nahrungsmittel enthalten Antioxidationsmittel und andere Stoffe, die natürlicherweise Blutgefäßwachstum verhindern.
- Regelmäßige Bewegung kann auch zur Vermeidung von AMD beitragen.

(English) Diabetic Macular Edema
(English) Diabetic macular edema (DME) is a form of diabetic retinopathy and a leading cause of vision loss in patients with DR.26, 27 It is characterized by swelling or thickening of the retina and the leaking of fluid, specifically in the macula,28 a small area in the back of the eye that focuses and sharpens vision.15

Prevalence
Globally, 21 million people are estimated to live with DME.20 Over 20% of people living with type 1 diabetes and 14-25% of people with type 2 diabetes (depending on their use of insulin) will develop DME within ten years.29, 30
Development of DME
DME is caused when fluid accumulates in the macula. It can develop without symptoms at any of the four stages of diabetic retinopathy, though it typically occurs in the more advanced forms. It is found in almost 50% of people with proliferative retinopathy, the advanced stage of DR.15
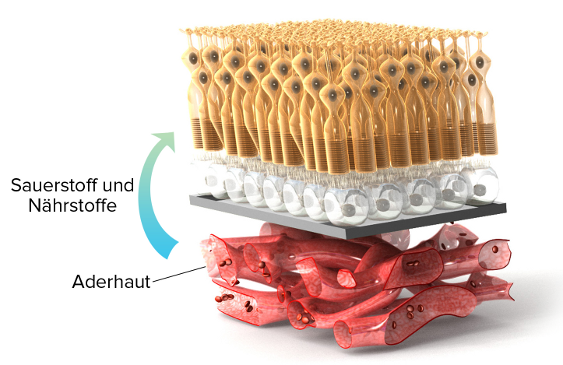
As was described in the development of diabetic retinopathy, high levels of blood glucose in diabetes patients cause damage to retinal blood vessels. This may deprive the retina of needed oxygen (a condition called hypoxia), which prompts an increase, or upregulation, in the glycoprotein VEGF (vascular endothelial growth factor). High levels of VEGF weaken the vessel wall and increase vascular permeability, which contributes to blood vessels becoming leaky.
As the vessels leak fluid and blood into the retina and, ultimately, the macula, the macula swells and thickens, resulting in macular edema.15
Swelling of the macula reduces visual acuity,31 the clarity or sharpness of vision at a distance, and blurs sight. If left untreated, DME can lead to severe and even permanent vision loss. When DME is treated in its early stages, vision loss can be delayed, stopped or, in some cases, even reversed.13

DME: TWO TYPES
There are two types of diabetic macular edema: focal and diffuse. However, there is no clear, consistent definition for these two types, and the classification and use of these terms has been inconsistent.32 It can be helpful to distinguish between focal and diffuse forms of DME because they may have different pathological processes, which would affect prognosis and predicting treatment outcomes24 for some therapies.
Focal
Focal macular edema is the most common and less severe form of DME.32 It is caused by changes in the structure of the retinal blood vessels, such as microaneurysms33 or dilated capilleries,32, 34 that leak fluid into a smaller area of the macula and do not involve the center of the macula.32 Because edema is limited, visual acuity does not decrease as much as it does in the diffuse form.
Diffuse
Diffuse macular edema is a less common but more severe form of DME that can be difficult to manage.24 It occurs when small capillaries in and around the macula leak fluid throughout most of the macula,34 including its center.32 As a result, most of the macula is thickened and visual acuity is more greatly reduced.32 The risk of developing diffuse macular edema increases with the severity of diabetic retinopathy.28
(English) Risk Factors: Diabetic Retinopathy & DME
(English) A risk factor is anything that affects your chances of getting a disease. Research has focused on risk factors for diabetic retinopathy so there has been little examination of risk factors specific to DME.24 However, diabetic retinopathy and DME both develop as a complication of diabetes and have similar risk factors.
If you have diabetes, you should get a comprehensive dilated eye exam every year. See the Testing section for more info.
(High levels of blood glucose)
Studies have shown that keeping glycemic levels as close to normal as possible can delay or prevent the development of DR.6, 39, 40, 41
(Abnormal levels of blood lipids)
(High blood pressure)
Hypertension-associated end-organ damage is a risk factor specific to DME.35
(Kidney disease)
Addressing the risk factors is the best way to slow or halt progression of either disease, which may occur without any changes to vision until it is too late to treat the condition. Diabetic retinopathy and DME rarely have visual symptoms in their early development and vision loss can occur very suddenly, so it is important to get regular screenings before symptoms appear.13
(English) Monitoring & Symptoms
(English)

Diabetic retinopathy develops without early symptoms or causing pain.15 Even in the advanced stages, proliferative retinopathy may not cause symptoms.15 Macular edema can develop at any stage of diabetic retinopathy without affecting vision.15 It is important not to wait for symptoms. Get tested before any issues with vision occur.

If blood vessels bleed into the eye, you may see blind spots in your vision. The spots may clear temporarily, but bleeding may reoccur and damage vision if the condition is left untreated. You may also experience blurry vision, or colors may look “washed out” or faded.55 Go see an eye care professional at the first sign of any of these symptoms.

In its early stages, diabetic retinopathy can be treated and vision can be preserved.19 If you do not receive treatment, diabetic retinopathy may progress into the proliferative form. Macular edema can also develop without symptoms and, if timely treatment is not obtained, DME may result in severe vision loss.
Early detection and timely treatment can save your vision. Learn How:
What You Can Do
As a person with diabetes, regular maintenance and regulation of your condition should be an integral part of daily life. There are steps that you can take to prevent or delay vision loss, and manage your condition and treatment:56
-
Regular Screening:
Get a comprehensive dilated eye exam at least once a year.It is recommended that people aged ten years or older with type 1 diabetes have a comprehensive eye exam within five years of the diagnosis, and that people with type 2 diabetes get a comprehensive eye exam as soon as they are diagnosed. Both type 1 and 2 diabetes patients should continue to receive subsequent eye exams on an annual basis.15,16 Less frequent exams may be an option after successful completion of one or more normal eye exams. If diabetic retinopathy is progressing, exams may be more frequent.16
Work with your eye care specialist to assess the best frequency of exams in order to manage your condition and prevent, or slow down, disease progression.
-
Control Blood Glucose:
HbA1c levels are a long-term measure of blood glucose control. HbA1c is a molecule that is formed when hemoglobin, a protein in red blood cells, connects to glucose.37 If there is more glucose in the blood to connect with hemoglobin, then more HbA1c will form.Keep your blood glucose levels as close to normal as you can.1 Hyperglycemia initiates many other risk factors, so controlling blood glucose can prevent other diabetic complications and slows down or even prevents the development of retinopathy.15
Discuss with your doctor about how best to control blood glucose levels.
-
Control Blood Pressure:
Studies have demonstrated that keeping your blood pressure as close to normal as possible reduces the risk of complications in the microvascular system by roughly 33%.1
Typically, the goal is to maintain a consistent blood pressure < 130/80 or below the 90th percentile for age, sex, and height (whichever number is lower).16
You can find more information on healthy blood pressure levels specific to age, sex and height at: www.nhlbi.nih.gov/health/prof/heart/hbp/hbp_ped.pdf -
Control Blood Lipids:
Keeping your cholesterol levels as close to normal as possible reduces risk of complications.1 High levels of total cholesterol or triglycerides can increase the risk of developing DME by two- or three-fold.57

(English) Testing
(English) If you have type 1 or type 2 diabetes, you should get a comprehensive eye exam at least once a year to screen for diabetic retinopathy and diabetic macular edema.
An ophthalmologist or optometrist who is experienced in diagnosing, managing and treating DR and DME is best suited to conduct these exams.16
A comprehensive eye exam typically includes a dilated eye exam, visual acuity test and tonometry. These tests can detect early signs of DR or DME, such as:15
- Retinal blood vessels that leak
- Damage or any change to the blood vessels
- Swelling or thickening of the retina
Types of Tests
A comprehensive eye exam includes:
1. Dilated Eye Exam
During a dilated eye exam, you will receive eye drops that dilate your pupils. This allows your eye specialist to see what is happening inside your eyes. Using a magnifying lens, your eye specialist will assess your retina and optic nerve to find any potential problems. If you have diabetes, it is important to receive this test at least once a year.15
2. Visual Acuity Test
This test uses an eye chart to measure your vision at various distances.15
3. Tonometry
This test measures the pressure in your eye(s) and may use numbing drops.15
4. Fluorescein angiogram (FA)
This test is taken when presence of DME is suspected. A certain type of dye will be injected into your arm and will pass through your blood vessels. This dye allows pictures to be taken of the retinal blood vessels so your eye care professional can detect any vessels that leak. If DME is found, work with your eye care specialist to determine the best treatment.15
5. Optical Coherence Tomography (OCT)
OCT is another tool that tests for DME. It is a certain type of camera that photographs and measures the thickness of your retina. It is also effective at detecting any swelling and fluid in the retina.58 The benefit of OCT is that it is non-invasive. Also, it makes it possible to evaluate treatment response more objectively.33
When to Get Tested16
Type 1 Diabetes
Patients with type 1 diabetes aged ten years or older should have their first comprehensive dilated eye exam within 5 years of developing diabetes.
Type 2 Diabetes
Patients with type 2 diabetes should have their first comprehensive dilated eye exam as soon as their diabetes is diagnosed.
Both type 1 and 2 diabetes patients should continue to receive subsequent eye exams on an annual basis. Less frequent exams may be an option after successful completion of one or more normal eye exams. Exams will be more frequent if retinopathy is progressing. Work with your ophthalmologist or optometrist to identify the best frequency of testing for you.
If you are diagnosed with severe nonproliferative diabetic retinopathy, proliferative diabetic retinopathy, or DME, go see an eye specialist experienced in treating and managing these conditions.
(English) Understanding VEGF & Macular Edema
(English) What Is VEGF?
The vascular endothelial growth factor (VEGF) is a glycoprotein that has been found to contribute significantly to the development of diabetic macular edema. VEGF plays an important role in many processes in the body, but excessively high levels of VEGF can have harmful effects.
VEGF & DME
Excessively high levels of VEGF have been found in retinopathy59 and DME.61 When retinal blood vessels become weak or blocked in diabetic retinopathy, the retina cannot receive enough blood or oxygen (hypoxia) and sends signals to the body for nourishment. VEGF is then released in the retina at abnormally high levels, which increases vascular permeability. This contributes to the rupture of the blood vessel wall and consequential swelling of the vessels,33, 60 resulting in damaged vessels that leak33 fluid into the central retina. As fluid accumulates in the macula, the macula swells and thickens, resulting in swelling of the macula and, ultimately, DME.
Research has shown that over-expression of VEGF plays a significant role in DME61 and is an important target for treating the condition.
(English) Patient Perspective
(English)
Ang-2 Webinar
The Angiogenesis Foundation has published a new Webinar Series on Vascular Stabilization in Retina Health and Disease to provide the vision community and clinicians treating retinal vascular eye diseases with an up to date overview of the Angiopoietin-Tie Pathway, and how this pathway is involved in retinal health and disease.

Webinar speakers include: Max Gomez, PhD, Charles Wykoff MD, PhD, David Eichenbaum, MD, and Ramin Tadayoni, MD, PhD. Watch now: https://www.scienceofang2.org/webinar