Introduction
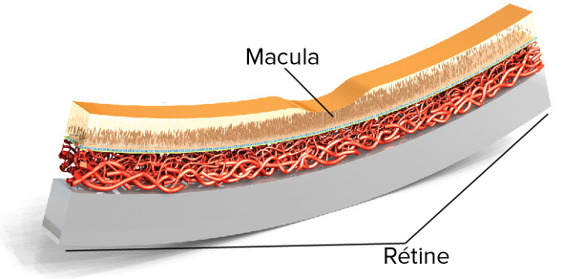
La dégénérescence maculaire liée à l’âge (DMLA) est la principale cause de cécité au-delà de 50 ans dans les pays développés et touche plus de 30 millions de personnes dans le monde. La DMLA est caractérisée par la perte de la vision centrale consécutive à la détérioration progressive de la « macula » – la partie de l’œil responsable de l’acuité visuelle, c’est-à-dire celle qui vous permet de voir les détails fins – et de la vision centrale. Avec la DMLA, il devient difficile de pratiquer des activités quotidiennes aussi précieuses que lire, conduire, reconnaître les visages, regarder la télévision et pouvoir emprunter un escalier sans encombre.
La DMLA est indolore et son évolution est variable – elle peut progresser aussi bien lentement que rapidement – et elle peut se limiter à un seul œil ou toucher les deux yeux. Lorsque le développement de la DMLA consiste en une baisse très progressive de la vision, dans un premier temps le cerveau est capable de compenser celle-ci, ce qui a pour effet de masquer les symptômes et de retarder leur identification. En cas de progression rapide, celle-ci peut s’accompagner d’une perte d’acuité visuelle dont le patient prend vite conscience. Quelle que soit la rapidité avec laquelle évolue la maladie, la DMLA non traitée peut conduire à une perte définitive de la vue.
Il existe deux formes de DMLA : la forme sèche et la forme humide.
Diabetes
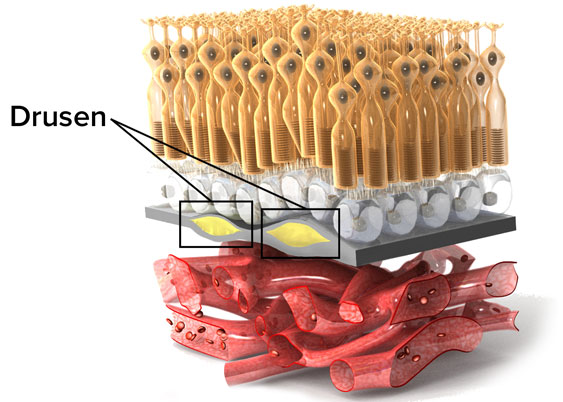
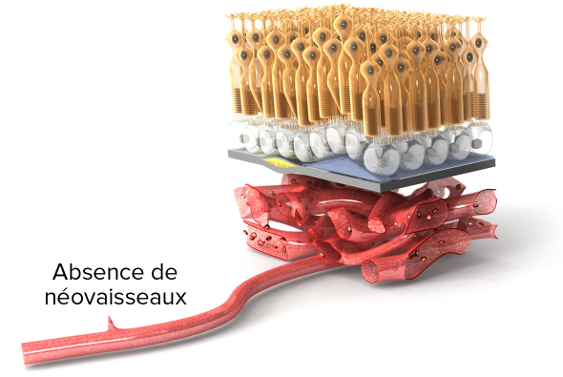
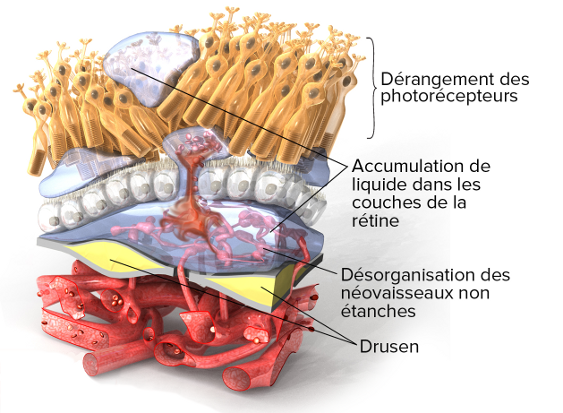
La DMLA sèche, ou atrophique, est la forme de DMLA la plus fréquente, dont les stades précoce et intermédiaire représentent environ 90 % de l’ensemble des cas. Au stade précoce de la DMLA sèche, on observe un déclin de la fonction de la macula, associé à l’accumulation de « drusen » (ou druses), c’est-à-dire de dépôts jaunâtres dans la partie postérieure de l’œil, variables en taille et en nombre ; cette accumulation est considérée comme faisant partie intégrante du processus de vieillissement de l’œil. À ce stade précoce de la DMLA sèche, les drusen peuvent être de faible dimension et présents en grand nombre ou moins nombreux mais de taille moyenne et l’on ne constate pas de baisse de la vision. La DMLA sèche précoce peut évoluer vers le stade intermédiaire, avec la multiplication des drusen de faible dimension ou le développement d’un ou plusieurs drusen plus volumineux. Les symptômes qui font leur apparition au stade intermédiaire de la DMLA sèche sont la présence de zones d’ondulation ou de flou au centre de la vision et une difficulté à lire.
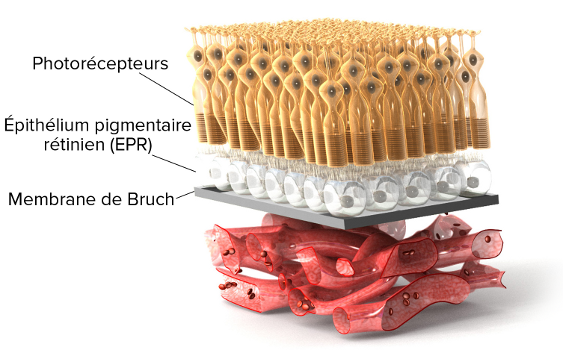
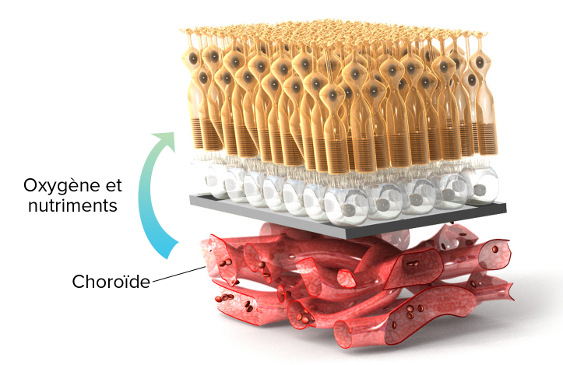
La DMLA sèche intermédiaire peut évoluer vers une DMLA sèche avancée ou vers une DMLA humide. Dans la DMLA sèche avancée, l’augmentation progressive du nombre et/ou du volume des drusen s’accompagne, au niveau de la macula, de la détérioration des photorécepteurs – cellules spécialisées dans la captation des signaux lumineux – et du tissu avoisinant ; c’est ce qu’on appelle « l’atrophie géographique ». L’atrophie géographique entraîne des troubles visuels plus importants et irréversibles comme la présence d’une tache plus large et plus sombre au centre de la vision, une diminution de la sensibilité aux contrastes, une difficulté d’adaptation aux changements d’éclairage (par exemple lors du passage d’un éclairage vif à un éclairage plus tamisé) et des difficultés à déchiffrer les petits caractères.
La DMLA sèche peut affecter un seul œil ou les deux yeux. Lorsqu’un seul œil est touché, la perte de vision est plus difficile à détecter car le « bon » œil travaille plus intensément pour compenser la déficience de l’œil atteint. C’est pourquoi il est important de se soumettre à des examens ophtalmologiques réguliers afin de faire contrôler l’acuité visuelle des deux yeux.
Diabetic Retinopathy
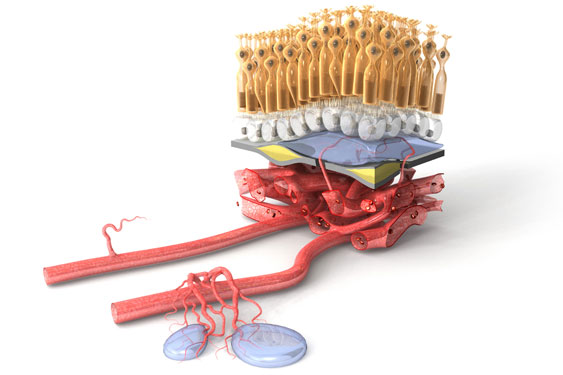
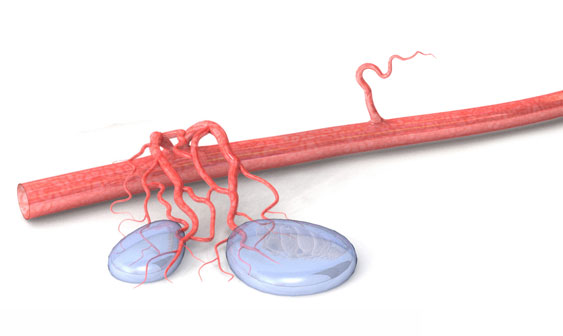
La DMLA humide est la forme la plus grave et la plus sévère de la DMLA ; elle ne se manifeste qu’à un stade avancé de la maladie. Alors que le développement d’une DMLA humide constitue systématiquement une aggravation d’une DMLA sèche préexistante, seuls 10 à 15 % des cas de DMLA sèche évoluent vers la forme humide. Également appelée « dégénérescence maculaire exsudative ou néovasculaire », la DMLA humide est caractérisée par la prolifération sous la macula de vaisseaux sanguins anormaux d’où il peut s’échapper du sang ou du liquide.
À la différence de la forme sèche de la DMLA, dont le développement est lent et progressif, la DMLA humide peut rapidement endommager la macula et provoquer une perte brutale de la vision centrale. C’est pourquoi il est extrêmement important que les patients à haut risque de DMLA humide se soumettent régulièrement à un examen de la vue.
Dans la DMLA humide, la prolifération anormale de vaisseaux sanguins au-dessous de la macula est le résultat d’un processus appelé « angiogenèse ». Ces vaisseaux anormaux laissent échapper du liquide et du sang susceptibles d’entraîner la formation, sous la macula, d’une poche en forme de bulle. Ces bulles déforment la vision de l’œil atteint, les lignes droites semblant alors onduler. Le patient peut percevoir une ou plusieurs taches sombres au centre de sa vision. Ce phénomène est dû à l’accumulation (ou collection) de sang ou de liquide sous la macula.
En l’absence de traitement, les hémorragies intraoculaires qui accompagnent la DMLA humide peuvent induire la formation de tissu cicatriciel, conduisant à la perte irréversible de la vision. Il y a toutefois une bonne nouvelle : il existe pour la DMLA humide différentes options thérapeutiques efficaces. Ces traitements sont capables de stabiliser la perte de la vision, voire de l’inverser dans certains cas, à condition d’être mis en œuvre avant que ne se forme le tissu cicatriciel.
Stages
Plusieurs facteurs peuvent vous exposer au risque de développer une DMLA :
- L’âge est le principal facteur de risque. Les plus de 60 ans sont les plus exposés.
- Si une DMLA a été diagnostiquée chez un membre de votre famille proche, votre risque de développer la maladie s’en trouve accru.
- Si l’un de vos yeux est atteint de DMLA, le risque que vous développiez une DMLA dans l’autre œil est important.
- Les fumeurs sont deux à trois fois plus susceptibles de développer une DMLA. Plus vous fumez, plus le risque est élevé.
- Cesser de fumer réduit le risque d’apparition d’une DMLA.
- Les femmes sont davantage exposées que les hommes au risque de développer une DMLA.
- La DMLA est plus fréquente dans les populations de type européen (également connues sous la dénomination scientifique de « populations de type caucasien ») que dans les populations d’origine africaine.
- L’obésité favorise l’évolution de la DMLA de types précoce et intermédiaire vers la DMLA avancée.
- Une hypertension artérielle non contrôlée augmente le risque de développer une DMLA.
Que puis-je faire pour réduire le risque de DMLA ?
- Abstenez-vous de fumer
- Veillez à maintenir votre poids de forme
- Surveillez votre tension artérielle
- Une alimentation riche en légumes à feuilles vertes et en fruits réduit le risque de développer une DMLA. La consommation régulière de poisson et de graisse de poisson, avec restriction des matières grasses provenant d’autres sources, limite le risque. Ces aliments renferment des antioxydants et des substances dotés de propriétés naturellement protectrices contre l’angiogenèse anormale.

- La pratique régulière d’une activité physique diminue le risque d’apparition d’une DMLA.
(English) Diabetic Macular Edema
(English) Diabetic macular edema (DME) is a form of diabetic retinopathy and a leading cause of vision loss in patients with DR.26, 27 It is characterized by swelling or thickening of the retina and the leaking of fluid, specifically in the macula,28 a small area in the back of the eye that focuses and sharpens vision.15

Prevalence
Globally, 21 million people are estimated to live with DME.20 Over 20% of people living with type 1 diabetes and 14-25% of people with type 2 diabetes (depending on their use of insulin) will develop DME within ten years.29, 30
Development of DME
DME is caused when fluid accumulates in the macula. It can develop without symptoms at any of the four stages of diabetic retinopathy, though it typically occurs in the more advanced forms. It is found in almost 50% of people with proliferative retinopathy, the advanced stage of DR.15
As was described in the development of diabetic retinopathy, high levels of blood glucose in diabetes patients cause damage to retinal blood vessels. This may deprive the retina of needed oxygen (a condition called hypoxia), which prompts an increase, or upregulation, in the glycoprotein VEGF (vascular endothelial growth factor). High levels of VEGF weaken the vessel wall and increase vascular permeability, which contributes to blood vessels becoming leaky.
As the vessels leak fluid and blood into the retina and, ultimately, the macula, the macula swells and thickens, resulting in macular edema.15
Swelling of the macula reduces visual acuity,31 the clarity or sharpness of vision at a distance, and blurs sight. If left untreated, DME can lead to severe and even permanent vision loss. When DME is treated in its early stages, vision loss can be delayed, stopped or, in some cases, even reversed.13

DME: TWO TYPES
There are two types of diabetic macular edema: focal and diffuse. However, there is no clear, consistent definition for these two types, and the classification and use of these terms has been inconsistent.32 It can be helpful to distinguish between focal and diffuse forms of DME because they may have different pathological processes, which would affect prognosis and predicting treatment outcomes24 for some therapies.
Focal
Focal macular edema is the most common and less severe form of DME.32 It is caused by changes in the structure of the retinal blood vessels, such as microaneurysms33 or dilated capilleries,32, 34 that leak fluid into a smaller area of the macula and do not involve the center of the macula.32 Because edema is limited, visual acuity does not decrease as much as it does in the diffuse form.
Diffuse
Diffuse macular edema is a less common but more severe form of DME that can be difficult to manage.24 It occurs when small capillaries in and around the macula leak fluid throughout most of the macula,34 including its center.32 As a result, most of the macula is thickened and visual acuity is more greatly reduced.32 The risk of developing diffuse macular edema increases with the severity of diabetic retinopathy.28
(English) Risk Factors: Diabetic Retinopathy & DME
(English) A risk factor is anything that affects your chances of getting a disease. Research has focused on risk factors for diabetic retinopathy so there has been little examination of risk factors specific to DME.24 However, diabetic retinopathy and DME both develop as a complication of diabetes and have similar risk factors.
If you have diabetes, you should get a comprehensive dilated eye exam every year. See the Testing section for more info.
(High levels of blood glucose)
Studies have shown that keeping glycemic levels as close to normal as possible can delay or prevent the development of DR.6, 39, 40, 41
(Abnormal levels of blood lipids)
(High blood pressure)
Hypertension-associated end-organ damage is a risk factor specific to DME.35
(Kidney disease)
Addressing the risk factors is the best way to slow or halt progression of either disease, which may occur without any changes to vision until it is too late to treat the condition. Diabetic retinopathy and DME rarely have visual symptoms in their early development and vision loss can occur very suddenly, so it is important to get regular screenings before symptoms appear.13
(English) Monitoring & Symptoms
(English)

Diabetic retinopathy develops without early symptoms or causing pain.15 Even in the advanced stages, proliferative retinopathy may not cause symptoms.15 Macular edema can develop at any stage of diabetic retinopathy without affecting vision.15 It is important not to wait for symptoms. Get tested before any issues with vision occur.

If blood vessels bleed into the eye, you may see blind spots in your vision. The spots may clear temporarily, but bleeding may reoccur and damage vision if the condition is left untreated. You may also experience blurry vision, or colors may look “washed out” or faded.55 Go see an eye care professional at the first sign of any of these symptoms.

In its early stages, diabetic retinopathy can be treated and vision can be preserved.19 If you do not receive treatment, diabetic retinopathy may progress into the proliferative form. Macular edema can also develop without symptoms and, if timely treatment is not obtained, DME may result in severe vision loss.
Early detection and timely treatment can save your vision. Learn How:
What You Can Do
As a person with diabetes, regular maintenance and regulation of your condition should be an integral part of daily life. There are steps that you can take to prevent or delay vision loss, and manage your condition and treatment:56
-
Regular Screening:
Get a comprehensive dilated eye exam at least once a year.It is recommended that people aged ten years or older with type 1 diabetes have a comprehensive eye exam within five years of the diagnosis, and that people with type 2 diabetes get a comprehensive eye exam as soon as they are diagnosed. Both type 1 and 2 diabetes patients should continue to receive subsequent eye exams on an annual basis.15,16 Less frequent exams may be an option after successful completion of one or more normal eye exams. If diabetic retinopathy is progressing, exams may be more frequent.16
Work with your eye care specialist to assess the best frequency of exams in order to manage your condition and prevent, or slow down, disease progression.
-
Control Blood Glucose:
HbA1c levels are a long-term measure of blood glucose control. HbA1c is a molecule that is formed when hemoglobin, a protein in red blood cells, connects to glucose.37 If there is more glucose in the blood to connect with hemoglobin, then more HbA1c will form.Keep your blood glucose levels as close to normal as you can.1 Hyperglycemia initiates many other risk factors, so controlling blood glucose can prevent other diabetic complications and slows down or even prevents the development of retinopathy.15
Discuss with your doctor about how best to control blood glucose levels.
-
Control Blood Pressure:
Studies have demonstrated that keeping your blood pressure as close to normal as possible reduces the risk of complications in the microvascular system by roughly 33%.1
Typically, the goal is to maintain a consistent blood pressure < 130/80 or below the 90th percentile for age, sex, and height (whichever number is lower).16
You can find more information on healthy blood pressure levels specific to age, sex and height at: www.nhlbi.nih.gov/health/prof/heart/hbp/hbp_ped.pdf -
Control Blood Lipids:
Keeping your cholesterol levels as close to normal as possible reduces risk of complications.1 High levels of total cholesterol or triglycerides can increase the risk of developing DME by two- or three-fold.57

(English) Testing
(English) If you have type 1 or type 2 diabetes, you should get a comprehensive eye exam at least once a year to screen for diabetic retinopathy and diabetic macular edema.
An ophthalmologist or optometrist who is experienced in diagnosing, managing and treating DR and DME is best suited to conduct these exams.16
A comprehensive eye exam typically includes a dilated eye exam, visual acuity test and tonometry. These tests can detect early signs of DR or DME, such as:15
- Retinal blood vessels that leak
- Damage or any change to the blood vessels
- Swelling or thickening of the retina
Types of Tests
A comprehensive eye exam includes:
1. Dilated Eye Exam
During a dilated eye exam, you will receive eye drops that dilate your pupils. This allows your eye specialist to see what is happening inside your eyes. Using a magnifying lens, your eye specialist will assess your retina and optic nerve to find any potential problems. If you have diabetes, it is important to receive this test at least once a year.15
2. Visual Acuity Test
This test uses an eye chart to measure your vision at various distances.15
3. Tonometry
This test measures the pressure in your eye(s) and may use numbing drops.15
4. Fluorescein angiogram (FA)
This test is taken when presence of DME is suspected. A certain type of dye will be injected into your arm and will pass through your blood vessels. This dye allows pictures to be taken of the retinal blood vessels so your eye care professional can detect any vessels that leak. If DME is found, work with your eye care specialist to determine the best treatment.15
5. Optical Coherence Tomography (OCT)
OCT is another tool that tests for DME. It is a certain type of camera that photographs and measures the thickness of your retina. It is also effective at detecting any swelling and fluid in the retina.58 The benefit of OCT is that it is non-invasive. Also, it makes it possible to evaluate treatment response more objectively.33
When to Get Tested16
Type 1 Diabetes
Patients with type 1 diabetes aged ten years or older should have their first comprehensive dilated eye exam within 5 years of developing diabetes.
Type 2 Diabetes
Patients with type 2 diabetes should have their first comprehensive dilated eye exam as soon as their diabetes is diagnosed.
Both type 1 and 2 diabetes patients should continue to receive subsequent eye exams on an annual basis. Less frequent exams may be an option after successful completion of one or more normal eye exams. Exams will be more frequent if retinopathy is progressing. Work with your ophthalmologist or optometrist to identify the best frequency of testing for you.
If you are diagnosed with severe nonproliferative diabetic retinopathy, proliferative diabetic retinopathy, or DME, go see an eye specialist experienced in treating and managing these conditions.
(English) Understanding VEGF & Macular Edema
(English) What Is VEGF?
The vascular endothelial growth factor (VEGF) is a glycoprotein that has been found to contribute significantly to the development of diabetic macular edema. VEGF plays an important role in many processes in the body, but excessively high levels of VEGF can have harmful effects.
VEGF & DME
Excessively high levels of VEGF have been found in retinopathy59 and DME.61 When retinal blood vessels become weak or blocked in diabetic retinopathy, the retina cannot receive enough blood or oxygen (hypoxia) and sends signals to the body for nourishment. VEGF is then released in the retina at abnormally high levels, which increases vascular permeability. This contributes to the rupture of the blood vessel wall and consequential swelling of the vessels,33, 60 resulting in damaged vessels that leak33 fluid into the central retina. As fluid accumulates in the macula, the macula swells and thickens, resulting in swelling of the macula and, ultimately, DME.
Research has shown that over-expression of VEGF plays a significant role in DME61 and is an important target for treating the condition.
(English) Patient Perspective
(English)
Ang-2 Webinar
The Angiogenesis Foundation has published a new Webinar Series on Vascular Stabilization in Retina Health and Disease to provide the vision community and clinicians treating retinal vascular eye diseases with an up to date overview of the Angiopoietin-Tie Pathway, and how this pathway is involved in retinal health and disease.

Webinar speakers include: Max Gomez, PhD, Charles Wykoff MD, PhD, David Eichenbaum, MD, and Ramin Tadayoni, MD, PhD. Watch now: https://www.scienceofang2.org/webinar